Jan 21 2026.
views 18By Kshalini Nonis
Ensuring that care homes are regulated and vulnerable residents are not exploited due to numerous young and middle-aged workers migrating overseas for employment, the question that arises is: who is left to care for our vulnerable older population? Whilst many elders/care homes are opening rapidly in Sri Lanka, some are run as a business. The state must act now to prevent unregulated institutions from exploiting vulnerable elders. We had a chat with Soshana Wijeratne Austin, Founder Director of the Kayden Cares Framework.
Q According to the Department of Census and Statistics, Sri Lanka has the fastest ageing population in South Asia, with 12.3 percent of the population being over 60 years in 2024. Therefore, who is there to take care of the elderly?
The Elders' Act of 2003 assumes that we, as a culture, continue to look after our elders and that only those who are financially disadvantaged are at risk. However, with increasing numbers of younger and middle-aged workers migrating overseas for employment, it is fair to question: Who is left to care for our vulnerable population?
Last year, it was reported that over 400,000 Sri Lankans left the country for overseas work. This reality highlights the urgent need for a safe, robust, sustainable, responsive, and effective social care system across both the public and private sectors.
Those who wish to remain in their own homes must be supported, whilst those who prefer to join a care community should have access to high-quality, regulated options. Equally important is the need to ensure that those delivering care are skilled, safe, standardised and responsive. The prevalence of illnesses such as dementia and chronic non-communicable conditions has increased dramatically. Further, we have a higher-than-average neurodivergent overpopulation.
Q What are your views on care homes that are opening up rapidly in Sri Lanka?
Sri Lanka’s care environment is expanding as families need help because of migration, smaller households, and a surge in dementia and long-term conditions. When governance lags, the most vulnerable carry the cost. Without clear standards, we see gaps in infection control, nutrition, medication safety, recordkeeping, and nighttime coverage. Complex needs—especially dementia—are being handled by untrained staff.
Four practical steps:
This is not an anti private sector. It’s pro quality. The majority of responsible providers want clear rules because it levels the playing field.
Q You said that some care homes are run as a business. Can you tell your reasons for saying this and how vulnerable residents are exploited in such homes?
“The care sector should be ‘profit with purpose.’ If services are not financially viable, they close. Run it like a business—but to standards.
Facts to Consider
Licensing must do two things: protect people and ensure sustainability. This means financial and continuity plans at registration, regular inspections (including unannounced), and a public register so families can verify a provider quickly.
Q There was a recent write-up in a National newspaper of one such home in Panadura. What action can be taken by the authorities about such institutes?
The recent tragedies—including the home where all the residents died when ‘Ditwah’ struck and another exposed as unregistered—prove we cannot leave elder care to chance. The state must act now: inspect every site, audit standards, and give providers a short, reasonable window to register and fix failures. High-risk homes should pause admissions immediately. If they still cannot meet standards, they must close.
Q You also said that Sri Lanka’s laws and policies have not kept pace with the evolving needs of older adults. What are your reasons for saying this?
What is critical in today’s elder environment is the loss of cognition and critical thinking. In the UK, especially after someone is diagnosed with dementia or over 80 years it is the responsibility of the solicitor/notary to test if the person understands the cause and effect of their decision to which they are attesting to. For every decision thereafter, this check needs to happen.
The Elders Act sets up a registry, not a modern safety net. We need up-to-date licensing, inspections, workforce standards, and safeguarding across home and residential care. We also need to have a system of checking, proving mental capacity for decisions regarding someone’s health and wellness, including their decision regarding their finances. We need an independent list with reviews from those receiving care, their families and friends.
Q With what authorities should such care homes, including the private ones, be registered?
An independent one. This is what the Kayden Cares Framework is about. We hope to create a practical pathway for any adult health social care service—residential homes, day centres, and home care agencies—to register, upskill, and comply with locally adapted standards grounded in international best practice.
The current legal framework (e.g., Protection of the Rights of Elders' Act, 2000/2011) establishes structures and registration but doesn’t provide a modern, enforceable standards code for staffing, training, dementia capable care, safeguarding, or continuity in case a service fails. The older Nursing Homes (Regulation) Act 1949, also doesn’t reflect today’s service models like assisted living or home care agencies—leaving gaps that our framework can help close while policy catches up.
Q Tell us why the Kayden Cares Framework was founded by you, based on your personal experience?
In Sri Lanka, my parents were subjected to an unchangeable “close circle” of live-in carers, suspected covert medication, repeated hypoglycaemic episodes, financial exploitation, and no transparent oversight that cut straight across the safeguards that should protect older adults and families. My mother’s human rights were violated when she was confined last year to an apartment with only a few visitors, and she was sedated as she was always sleeping when I called. This is cohesive control, and it is illegal in the international elder environment.
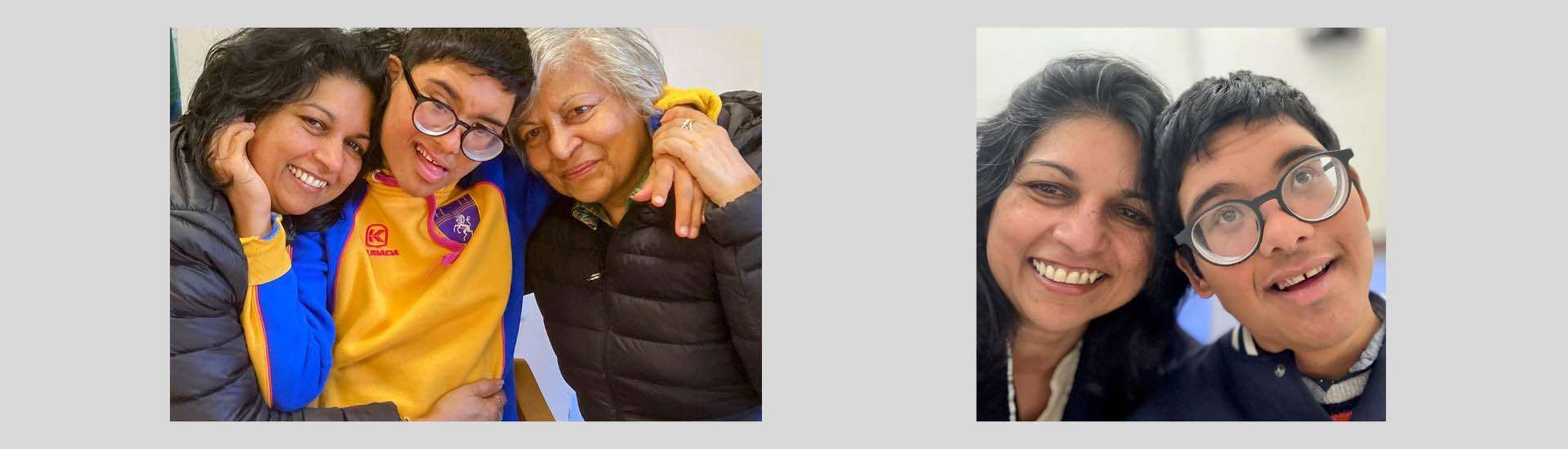
I had to take legal action to restore communication and eventually take my mother back to the UK with me, where she is happy, surrounded by those who love her- the family. I had nowhere to go with the cruelty and infringement on rights endured by my parents. No repeat prescription by a medical professional for the monthly purchasing of strong sedatives, insulin, and other diabetic medication and stool hardeners. Carers administering insulin without a medic's guidance, as my father’s food intake stopped. I want to return to Sri Lanka. I want my son, Kayden, to be safe to live here and for me to grow old with him.
Q How will the above-mentioned Framework address some of the issues discussed above?
I built Kayden Cares in the UK to provide the care that I believe is needed. In Sri Lanka, we do not need another care provider; what we need is learning from those who have treaded this road earlier and standards to guide the care that is delivered.
There are some very good examples of care in Sri Lanka that must be shared with others. This is what I intend to do with the Kayden Cares Framework here in Sri Lanka. It is an NGO that will deliver training, monitor and provide a place for families to find the right type of care for their loved ones. I appreciate the 87 policies my company in the UK has to practice.
My mother suffered repeated dangerous low sugar episodes; my father, with dementia, was left vulnerable; no health records were maintained, nor medication administered, and our complaints went nowhere.
Q How will this framework bridge the gap between Acts of Parliament and real-world care practices by providing the policy that is needed to guide care delivery, governance and advocacy for vulnerable elders?
This gap leaves many vulnerable to exploitation by those who view elder care as a business opportunity. It is the government’s duty to update and enforce laws that protect all citizens. It is also our collective responsibility to ensure that older adults are cared for with the full protection of their human rights. The Kayden Cares Framework was founded by me based on my own experience and commitment to ensuring that Sri Lanka becomes a country where my son, Kayden, can thrive—and where all of us can age safely and with dignity.
This framework bridges the gap between Acts of Parliament and real-world care practices by providing the bridging policy needed to guide care delivery, governance, and advocacy for vulnerable populations.
Their mission includes:
Q Can you tell us briefly about your soft launch?
Currently, we are registering and getting our IT system in place. We are researching and mapping the current environment. We are placed well to join the amazing activities of existing entities and bring about standardisation, training and assessment, making it easy for providers to know what they need to deliver and the public to be armed with the right knowledge, when making care decisions for their loved ones.
Sri Lanka’s systems are fantastic. Pertinent training must be the same for the carer profession and family information. We also need the private sector to invest in setting this up.
0 Comments